This collaborative research initiative, with partner sites in Erlangen, Berlin, Kiel, and Innsbruck, aims to gain groundbreaking insights into the complex interactions between the intestinal barrier and the immune system in chronic inflammatory bowel diseases (IBD). By bringing together leading experts in immunology, gastroenterology, and bioinformatics, the consortium fosters innovative and interdisciplinary research approaches.
The goal of this collaborative effort is not only to deepen our understanding of the underlying mechanisms of IBD but also to pave the way for the development of novel therapeutic strategies. These strategies are designed to enable more targeted and effective treatments that have the potential to significantly improve patients’ quality of life — and ultimately contribute to long-term remission or even a cure.
Through the combined expertise and resources of all participating institutions, the initiative also seeks to maximize research efficiency and accelerate progress toward future medical breakthroughs.
In summary, our research provides crucial and previously unattained insights into the dynamics of immune-epithelial communication in inflammatory bowel diseases (IBD). These profound findings have the potential to lay the foundation for a revolutionary concept in understanding the pathophysiology of IBD. Moreover, they open new avenues for the development of innovative therapeutic strategies specifically aimed at modulating the interactions between immune cells and the intestinal epithelium.
By translating these insights into clinical practice, tailored treatment approaches could emerge that are not only more effective but also associated with fewer side effects for patients. In the long term, these advances could lead to a significant improvement in the quality of life for affected individuals and bring about a paradigm shift in IBD therapy.
Our research thus stands at the threshold of groundbreaking developments with the potential to sustainably transform the landscape of medical science and patient care.
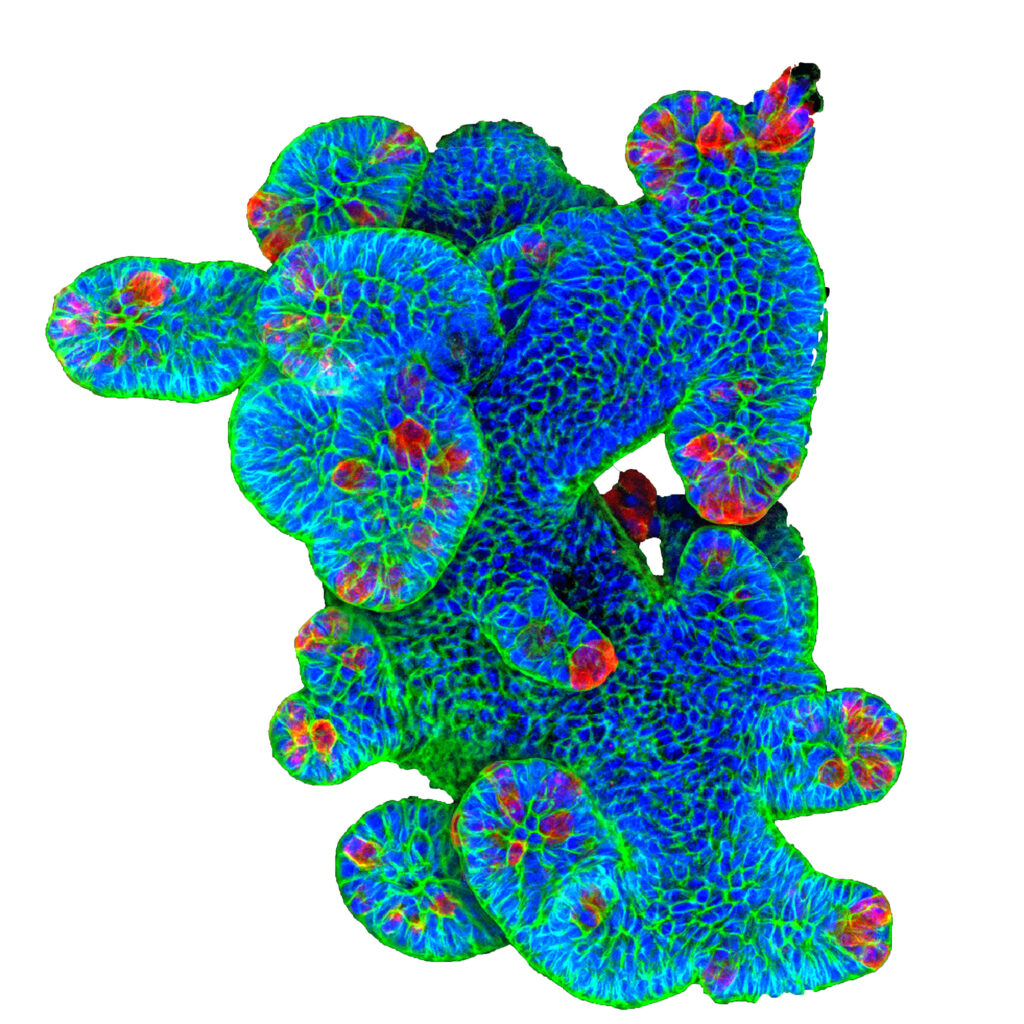
Chronic intestinal inflammation is often associated with increased activity of inflammatory markers, including certain cytokines such as interferons, TNF-α, IL-6, and IL-1β. These cytokines are known to activate the immune system and amplify inflammation. What is less well understood, however, is their effect on the cells lining the inside of our intestines, known as intestinal epithelial cells. Recent research has shown that cytokines like TNF-α, IL-22, and IL-33 are particularly important—not only because they influence inflammation in the gut, but also because they play a role in regulating the function of these epithelial cells.
It is becoming increasingly clear that these pro-inflammatory cytokines do not merely affect the immune system, but also act directly on the intestinal epithelial cells. Through this, they help maintain gut homeostasis and regulate the barrier function of the intestine—its ability to act as a protective wall. The epithelial cells themselves express various receptors for these cytokines, meaning they can receive both anti-inflammatory and pro-inflammatory signals.
The primary goal of Research Area A is to gain a deeper understanding of how signals from immune cells and other cells in the gut are transmitted to epithelial cells, and how this impacts the intestinal barrier. We aim to uncover how these interactions influence gut balance and protective functions.
Disrupted communication between intestinal epithelial cells and the immune system plays a key role in the development of inflammatory bowel diseases (IBD). Simply put, certain messenger molecules released by the immune system can disturb the function and balance of the intestinal epithelial cells. When these cells are stressed or their protective role is compromised, bacteria can cross the intestinal wall and trigger an immune response.
Furthermore, intestinal epithelial cells secrete signaling molecules that can influence the immune system within the gut, as well as substances that act against microbes, thereby shaping the composition of gut bacteria in both healthy and inflamed intestines. An interesting observation is that germ-free mice—raised in sterile environments without gut bacteria—also show an underdeveloped immune system. This highlights the crucial interplay between gut bacteria, intestinal cells, and the immune system.
The main objective of Research Area B is to understand how intestinal epithelial cells and their barrier functions influence and shape immune responses and inflammation in the gut during IBD.
A major breakthrough in drug development that has greatly improved IBD treatment is the introduction of biologics and new small molecules. These medications specifically target parts of the inflammatory process to suppress it. However, there are drawbacks, such as increased risk of infections and cancer, and about half of the patients treated with antibodies do not experience symptom improvement. This underscores the urgent need to identify new treatment targets and biomarkers that can predict whether a therapy will be effective for a given patient.
Discovering new therapeutic pathways can help us develop novel drugs and diagnostic methods, ultimately moving toward personalized medicine. In this new era, physicians will be able to predict which patients will respond to a particular treatment and which will not, thus avoiding unnecessary side effects.
Until now, new treatment strategies have mainly focused on the excessive activation of the immune system. However, with the growing recognition of the important role of the intestinal epithelium and its interactions with both gut bacteria and the immune system, we strive to explore how the disrupted communication between these systems can be harnessed for therapy.
The main goal of Research Area C is to discover new diagnostic and therapeutic approaches that target this disrupted communication. Our overarching research objective is to develop such innovative treatment and diagnostic methods and to evaluate them in clinical trials.